Navigating HAE
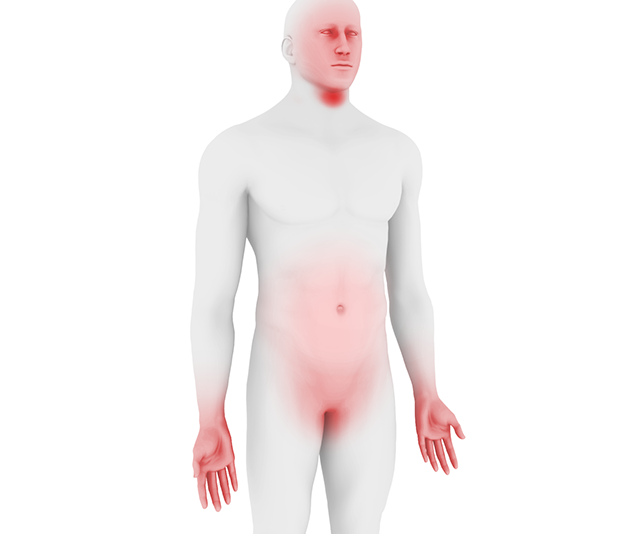
The condition is associated with a substantial and multifaceted burden of illness affecting various aspects of a patient's quality of life (e.g., emotional state, career and education progression, and the decision to have children).2,7,20,21,22,23,24 Types I/II are indistinguishable in their clinical presentation, having identical symptoms characterized by edema attacks that can vary in location, frequency, duration, and severity.1,25,26 Swelling and other symptoms gradually worsen over 12 to 36 hours, intensifying in a relentless manner, sometimes spreading to other sites, and then resolving over 2 to 5 days.7,14,27
A variety of possible triggers for attacks have been proposed, most commonly mechanical trauma, mental stress, and airway infection.2,4,28 Nevertheless, many attacks occur without an obvious trigger, particularly in children, highlighting the need for individualized treatment plans.2,4,19