

Digestive Disease Week® (DDW), 2026
Global meeting for physicians, researchers, and industry in the fields of gastroenterology, hepatology, endoscopy, and gastrointestinal surgery.
To report an adverse event or product quality complaint, call 1-877-TAKEDA-7 (1-877-825-3327)

Not an actual patient.
Population-based studies in the U.S. suggest that the incidence of IBD is most common in patients aged 15 to 35 years.1 IBD can also present in childhood, including up to 20% of children who are diagnosed before the age of 10 years.5 It is more common in Whites (vs other racial groups) and in adults, UC is more common in males.1,6
Symptoms of IBD depend on the disease location, and can range from mild to moderate to severe.2,4 Diarrhea and rectal bleeding are characteristic with UC. Patients can experience weight loss and fever (although it can be less common than with CD), and abdominal pain varies depending on the patient. For CD, weight loss, fever, and abdominal pain are more predominant, although these patients can also experience diarrhea and rectal bleeding.4
Irritable bowel syndrome (IBS), the most common GI condition diagnosed by gastroenterologists, may be mistaken for IBD since IBS symptoms may mimic those seen in a patient with mild IBD, but history and additional diagnostic tests can help rule it out of the differential diagnosis.7 Endoscopy combined with biopsies of the affected area(s) of the GI tract will also establish the diagnosis and differentiate between UC and CD.4,8
The etiology of IBD most likely involves a complex interaction between genetic and environmental factors, microbiome, and the immune system.3,4 T cells, which are activated by antigen-presenting cells in the peripheral lymphoid tissue, migrate to the site of inflammation and play a role in recruitment and activation of additional inflammatory cells in the GI tract.9,10
IBD is a chronic disease, with significant impact on a patient’s general health.3 While the Crohn’s Disease Activity Index (for CD) and Mayo Score (for UC) are the most frequently used instruments for scoring and monitoring disease activity in clinical trials, researchers are working to improve the measures of disease activity and severity through assessment of impact of disease on the patient, disease burden, and disease course, including structural damage with a goal of improving disease management for patients.11
This is not intended to be a comprehensive resource of all congresses and congress materials across therapeutic and disease areas. Congress materials may include information about investigational use(s) of compounds/products that are not approved for use by the U.S. Food and Drug Administration (FDA) and/or are inconsistent with the Prescribing Information. Takeda does not recommend the use of any Takeda product beyond the approved labeling. Any decisions regarding the usage of a Takeda product beyond the approved labeling are left to the discretion of the healthcare professional. Takeda makes no representations about whether investigational compounds or unapproved uses will be approved by the FDA.


Global meeting for physicians, researchers, and industry in the fields of gastroenterology, hepatology, endoscopy, and gastrointestinal surgery.


Annual global conference for interdisciplinary, clinical nutrition leaders, providing the latest in clinical nutrition research, education, and products.


Annual conference for a multidisciplinary community of practitioners and researchers focusing on inflammatory bowel disease (IBD) by pairing best practices in clinical care with innovative research.


An all-encompassing event providing real-world clinical education, case studies and new evidence-based approaches in IBD management.


Global meeting featuring thought leaders from around the world focused on advancing patient care in allergy and immunology.


Annual forum for participants to learn about the latest advances in pediatric gastroenterology, hepatology, and nutrition, and to discuss current topics in clinical applications.


Annual event with more than 2,500 members and non-members of the AMCP to engage on the latest innovations and most intentional networking in managed care pharmacy.


Premier event for clinicians and the general public about digestive disorders and the latest trends in GI technology and therapeutics.


The International Intestinal Rehabilitation and Transplantation Association (IIRTA) aims to serve its scientific community in providing a forum for open exchange of knowledge and expertise to promote intestinal rehabilitation and transplantation as a safe, innovative science involving nutritional, medical, surgical and transplant therapies through education, policy development and research. Every two years, the IIRTA brings together clinicians and scientists from all over the world in the fields of intestinal rehabilitation and transplantation.


Conference specifically designed by advanced practice providers (APPs) for the purpose of meeting the educational needs of APPs who specialize in the management of patients with GI disorders and chronic liver disease.


Leading global conference discussing how to establish, incentivize, and share value sustainable for health systems, patients, and technology developers.


Global meeting for physicians, researchers, and industry in the fields of gastroenterology, hepatology, endoscopy, and gastrointestinal surgery.


Annual global conference for interdisciplinary, clinical nutrition leaders, providing the latest in clinical nutrition research, education, and products.


Premier global educational event for allergists and immunologists, with thousands of attendees each year, discussing allergies, asthma, and immune deficiency disorders.
This resource provides information on Takeda medications available in the Inflammatory Bowel Disease category and is not intended to represent a complete list of therapeutic options.
(vedolizumab)
(mesalamine)
(mesalamine)
The prevalence of IBD in the U.S. is among the highest in the world.1 A 2023 epidemiology studied showed that the Northeast and South regions of the U.S. have higher rates of IBD compared to the West and Midwest.1,3,4 Additionally, prevalence is slightly higher in males among children and females among adults.1 There has been an observed significant rise in cases in the pediatric population, driven mainly by patients aged between 10 and 17 years old.5
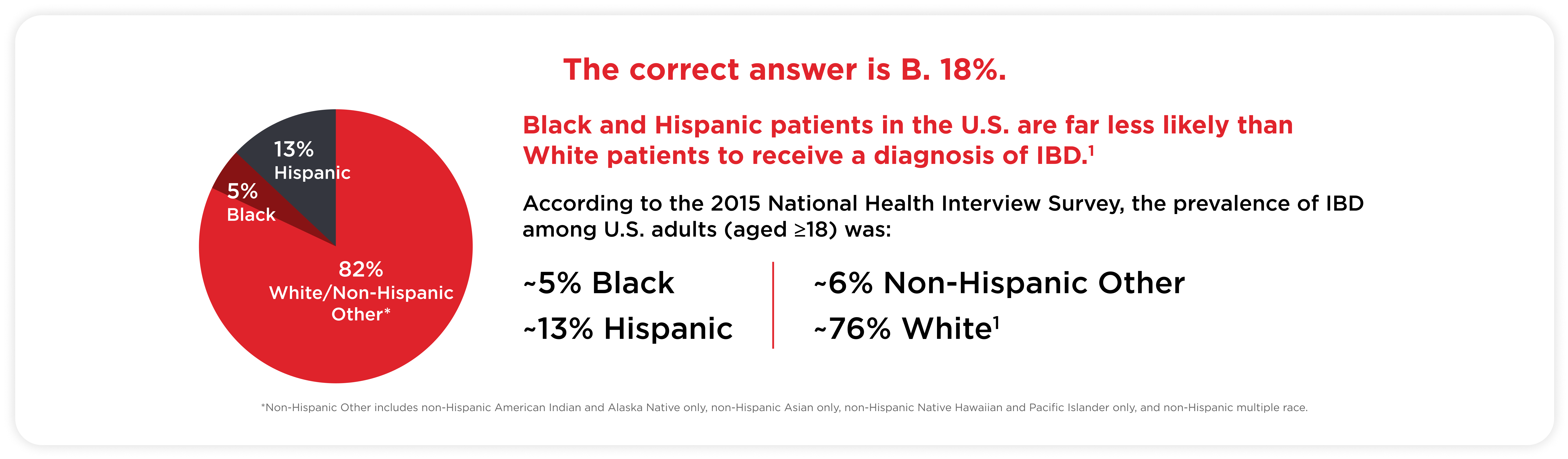
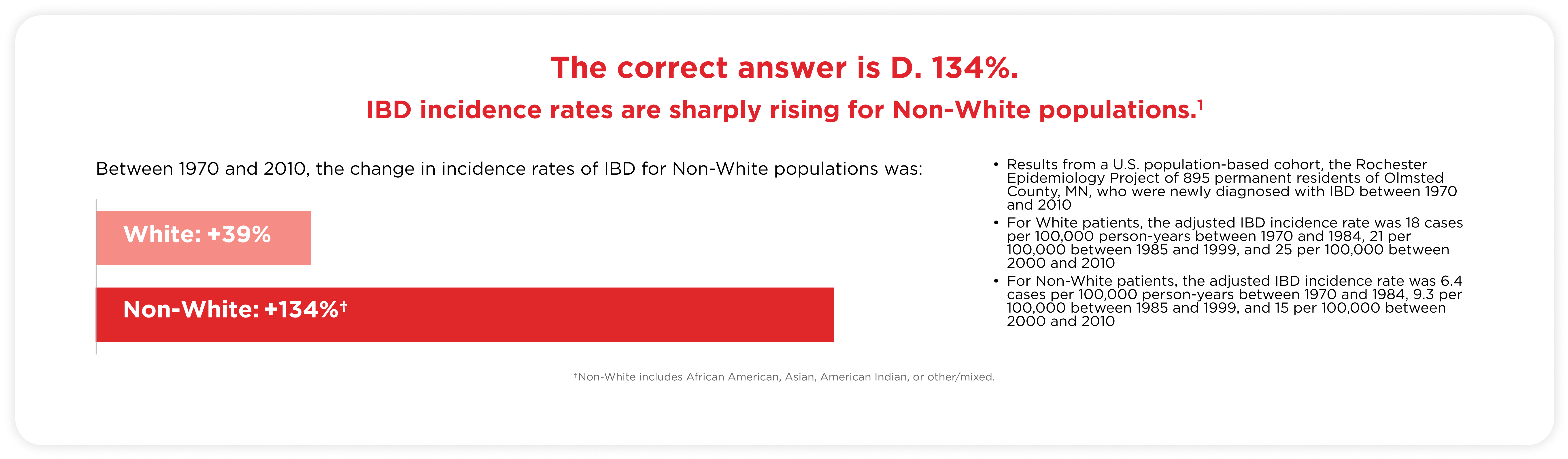
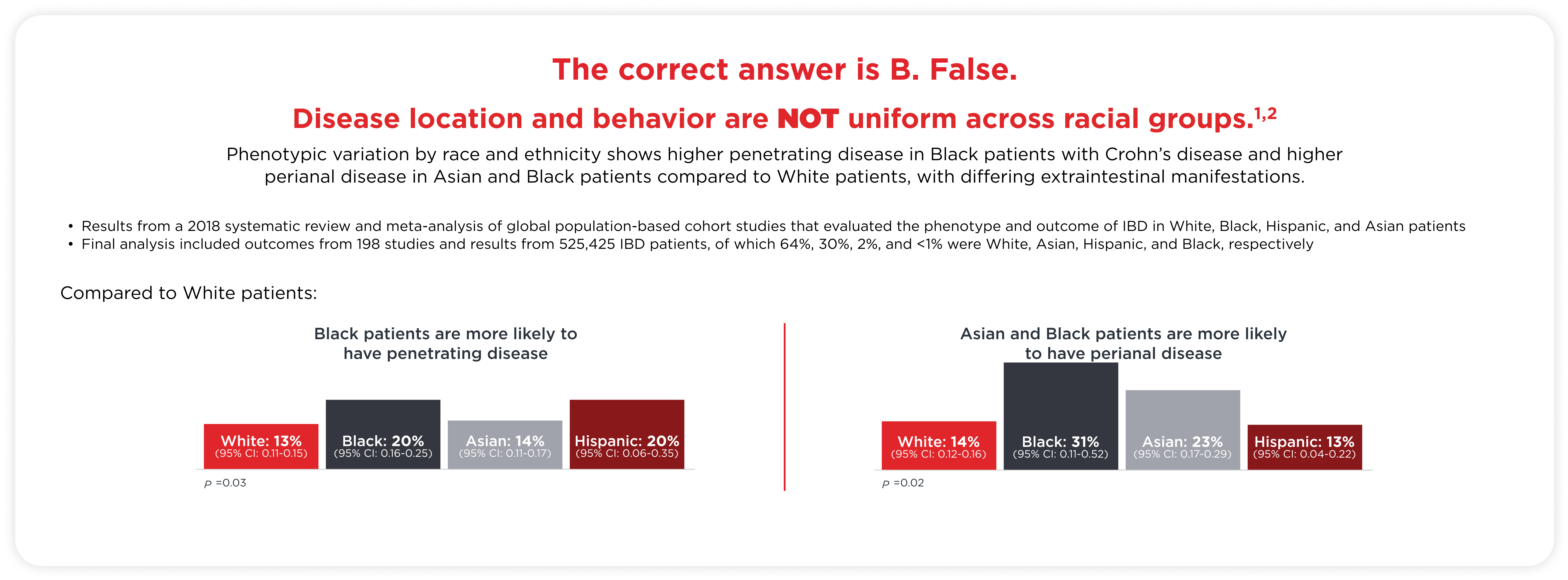
Incidence and prevalence rates of IBD are higher in White patients compared with patients of other races.1 However, a 2017 study demonstrated that between 1970 and 2010, there was an 39% increase in IBD incidence rates for White patients and 134% increase for patients of other races (African American, Asian, American Indian, and Other), suggesting that the future of IBD in the U.S. may experience a shift in racial diversity.6
The pathophysiology of IBD has yet to be fully defined but is known to include a combination of genetic, environmental, microbiological, and immunological factors.7-9 The interplay between these factors can compromise the intestinal mucosa and epithelial barrier. The subsequent influx of antigens and microorganisms into the lamina propria of the gut is associated with activation of the innate immune response, and a persistent, adaptive immune response.10-13
Symptoms of IBD depend on the disease location and can range from mild to moderate to severe.14 Common symptoms of CD include diarrhea, abdominal pain, and fatigue; weight loss, fever, growth failure, anemia, recurrent fistulas, or extraintestinal manifestations can also be presenting features.15 For UC, the main symptom is bloody diarrhea, with or without mucus; other symptoms include urgency or tenesmus, abdominal pain, malaise, weight loss, and fever, depending on the extent and severity of disease.16
Irritable bowel syndrome (IBS), the most common GI condition diagnosed by gastroenterologists, may be mistaken for IBD since IBS symptoms may mimic those seen in a patient with mild IBD, but history and additional diagnostic tests can help rule it out of the differential diagnosis.17 Diagnosis of IBD is a multistage process including physical examination and medical history, endoscopy, lab testing, and cross-sectional imaging.18
IBD can substantially compromise the physical, psychological, familial, and social dimensions of life, with secondary effects evident in the increased rates of anxiety, depression, and other emotional effects.20 As chronic IBDs, CD and UC can lead to disabling bowel symptoms and progressive bowel damage throughout a patient’s life, resulting in prominent disability, reduced quality of life, and increased morbidity.20,21 Patients with IBD expect to be informed about their disease, enabling shared decision making that ultimately leads to symptom control and improved quality of life.22
Find materials to help foster a deeper understanding of health equity in Inflammatory Bowel Disease.
IBD = inflammatory bowel disease
U.S. = United States
1. Dahlhamer JM, Zammitti EP, Ward BW et al. MMWR Morb Mortal Wkly Rep. 2016;65(42):1166-1169.
IBD = inflammatory bowel disease
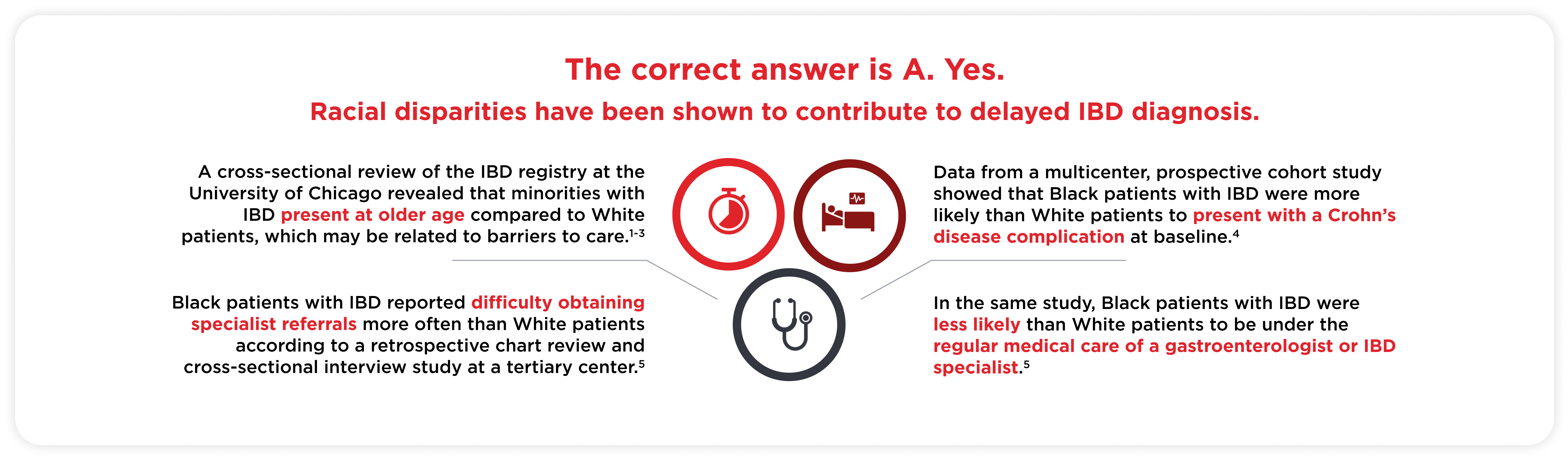
1. Odufalu FD, et al. Curr Opin Gastroenterol. 2022;38(4):321–327; 2. Sofia MA et al. Dig Dis Sci. 2014;59(9):2228–2235; 3. Damas OM et al. Am J Gastroenterol. 2013;108(2):231–239; 4. Barnes EL, et al. Inflamm Bowel Dis. 2018;24(12):2634–2640; 5. Nguyen GC, LaVeist TA, Harris ML et al. Am J Gastroenterol. 2010;105(10):2202–2208.
IBD = inflammatory bowel disease
MN = Minnesota
U.S. = United States
1. Aniwan S, Harmsen WS, Tremaine WJ et al. Therap Adv Gastroenterol. 2019 Feb 6;12:1756284819827692. doi: 10.1177/1756284819827692
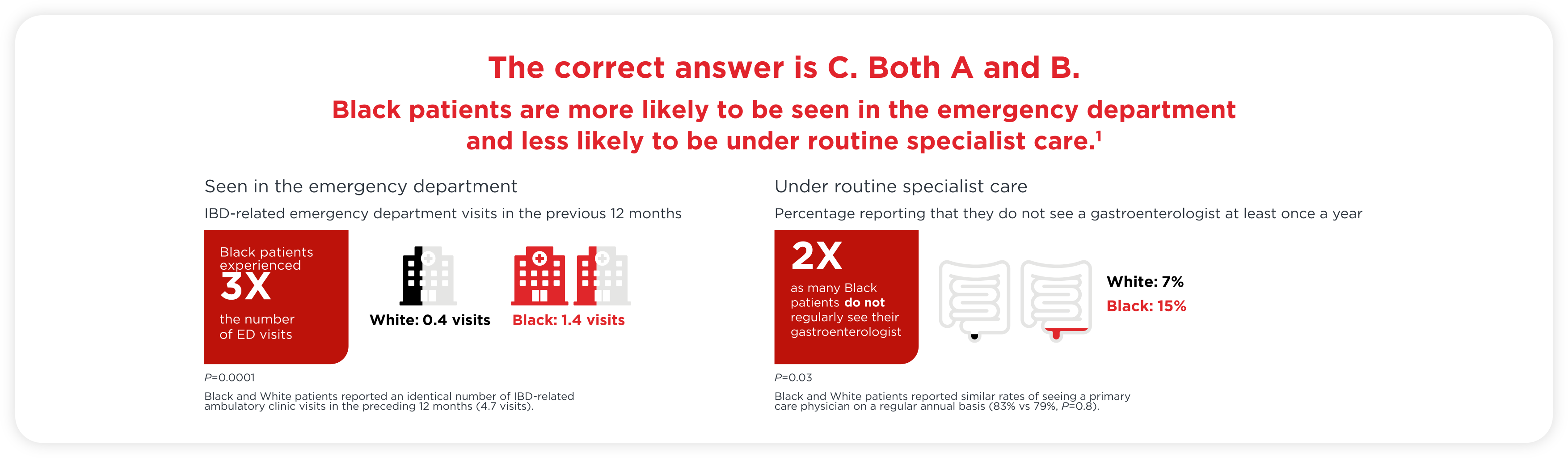
*Cross-sectional study included Black (n=137) and White (n=149) patients with IBD who were recruited from an outpatient IBD clinic in the U.S.
ED = emergency department
IBD = inflammatory bowel disease
U.S. = United States
1. Nguyen GC, LaVeist TA, Harris ML, et al. Am J Gastroenterol. 2010;105(10):2202–2208.
IBD = inflammatory bowel disease
1. Shi HY, Levy AN, Trivedi HD et al. Clin Gastroenterol Hepatol. 2018;16(2):190-197; 2. Louis E, Collard A, Oger AF et al. Gut. 2001;49(6):777-782.
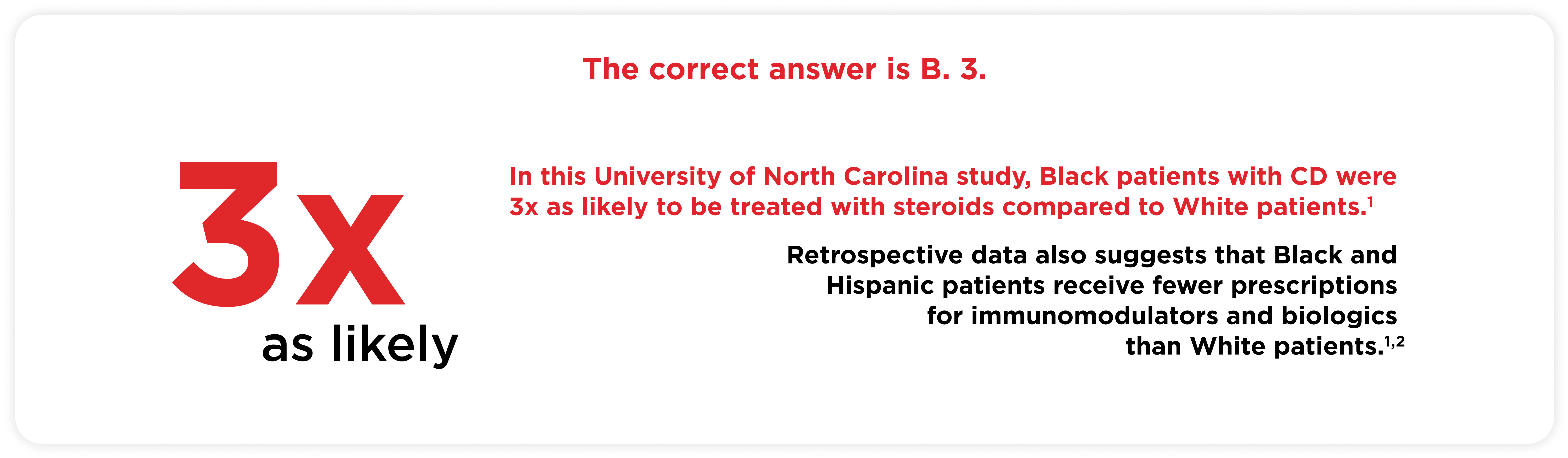
CD = Crohn's disease
1. Odufalu FD, et al. Curr Opin Gastroenterol. 2022 Jul 1;38(4):321-327; 2. Nguyen GC, LaVeist TA, Harris ML et al. Am J Gastroenterol. 2010 Oct;105(10):2202-2208,
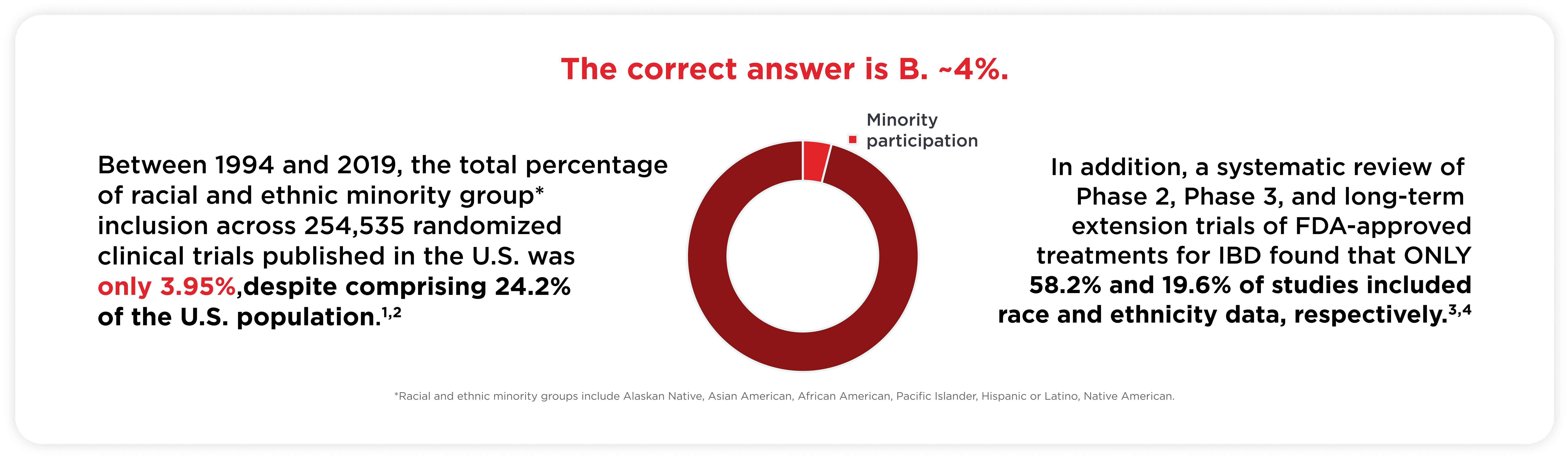
FDA = Food and Drug Administration
IBD = inflammatory bowel disease
U.S. = United States
1. Ma MA, Gutiérrez DE, Frausto JM, et al. Mayo Clin Proc. 2021;96:264–266; 2. United States Census Bureau. Quick facts. 2021. Accessed August 2024. https://www.census.gov/quickfacts/; 3. Cohen NA, Silfen A, Rubin DT. Gastroenterology. 2022;162:17–21; 4. Johnson C, Barnes EL, Zhang X, et al. Crohn's Colitis 360. 2020 Apr;2(2):otaa023. doi: 10.1093/crocol/otaa023.
©2025 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved.
TAKEDA and the TAKEDA logo are registered trademarks of
Takeda Pharmaceutical Company Limited.
Find materials to help foster a deeper understanding of Inflammatory Bowel Disease (IBD).
Learn more about inflammatory bowel disease (IBD), a chronic inflammatory, relapsing-remitting disease that includes two main subtypes, Crohn’s disease (CD) and ulcerative colitis (UC).